Antimicrobial resistance
With improved hygiene, more controls and more research, the German government’s German Antimicrobial Resistance Strategy (DART) aims to stem the spread of resistant pathogens, which are making it increasingly difficult to provide patients with effective treatment.
4 min reading time
The German government has put the issue of antimicrobial resistance on the agenda for the G7 summit
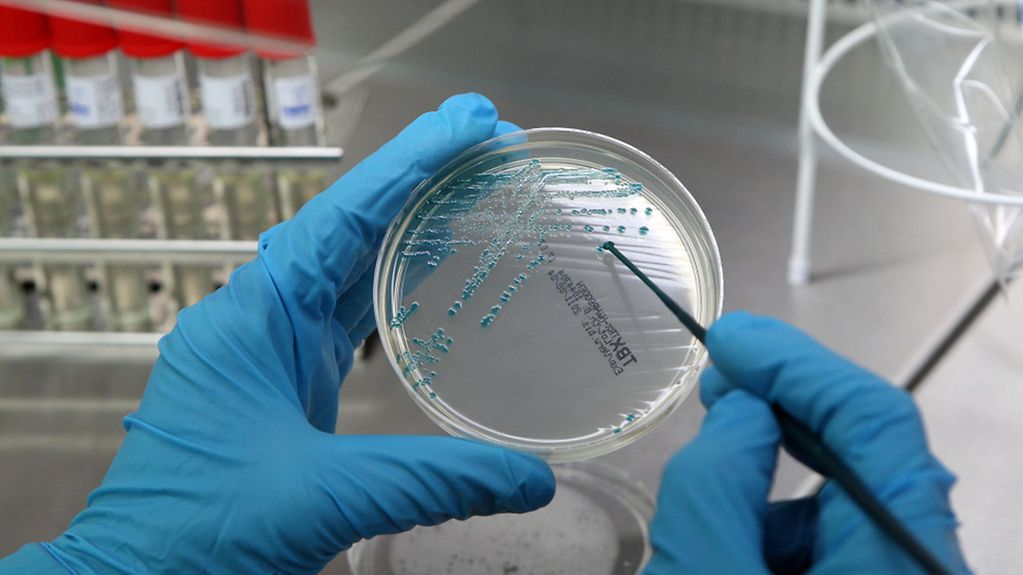
Photo: picture-alliance/dpa/Bernd Wüstneck
Every year between 400,000 and 600,000 people become infected in German hospitals. 10,000 to 15,000 of them die as a result. Increasingly the pathogens involved are resistant to antibiotics. Around the world we can see a rise in the prevalence of bacteria that are less sensitive to common antibiotics, or even totally resistant to these. Antibiotics are thus becoming less effective in the treatment of infectious diseases, which limits the treatment options available.
"If antibiotics no longer work, the treatment options available could be those of the pre-penicillin era, which would have dramatic consequences. Diseases that today are easily curable, like a bladder infection or a wound that becomes infected following surgery, could become serious health threats," warned Federal Health Minister Herrmann Gröhe.
Incorrect use of antibiotics in human and veterinary medicine, poor hygiene and the rise in international trade and travel help spread the resistant pathogens.
Preventing the spread of resistant bacteria
This is why the Cabinet adopted the German Antimicrobial Resistance Strategy - DART 2020. The aim is to take a ‘one health’ or overarching approach in order to stem the spread of resistant pathogens. Often animals and humans become infected with the same bacteria, and are treated with the same antibiotic. It is important that resistance be identified at an early stage, that treatment options are retained and infection chains broken.
"We need clear rules governing the use of antibiotics in medicine and stock farming, but we also need to forge ahead with research to develop new antibiotics, alternative treatment methods and tests permitting swift diagnoses," said Hermann Gröhe.
DART 2020 also outlines measures designed to better inform people about antimicrobial resistance and hygiene in hospitals.
The Davos World Economic Forum declared antimicrobial resistance to be one of the greatest risks for the global economy. The costs of treatment rise and patients die when antibiotic treatment fails.
Acting together at international level
The World Health Organization (WHO) is currently elaborating a Global Action Plan on Antimicrobial Resistance, which is to be adopted at the World Health Assembly in May 2015. One key element of the action plan is the development of national strategies. Germany is an example for others to follow. It was quick off the mark, and with DART 2020 it has responded to the calls of the WHO.
The German government has put the issue on the agenda of the G7 summit to be held at the beginning of June in Schloss Elmau. Scientists and non-governmental organisations have already consulted on the matter in dialogue forums in the lead-up to the G7 summit.
As the Federal Health Minister said, "No country in the world can alone stop the rise in antimicrobial resistance. That is why we must all pull together at international level."
Much achieved – but a lot of work lies ahead
In 2008 the German government published its first Antimicrobial Resistance Strategy. The initial achievements can already be seen: some resistant pathogen rates have been declining for years. Doctors are prescribing fewer antibiotics to in-patients, while figures for out-patients are stable.
In 2011 the Infection Protection Law was tightened up. As a result all of Germany’s federal states have adopted new hygiene regulations or modified existing ones. This is important in order to improve hygiene in health facilities. Regional networks have been put in place to prevent and control resistant infective agents. The Federal Ministry of Health has promoted a number of different pilot networks.
What exactly are antibiotics?
Antibiotics are naturally occurring antibodies and signals that trigger bacterial response. One of the first antibiotics to be used was penicillin, a mould that kills bacteria. Moulds and bacteria can produce different antibiotics, to defend themselves against other microorganisms. Alongside these antibiotics in the strictest sense of the term, synthetically manufactured chemotherapeutic agents are also termed antibiotics. Used even in small quantities, these substances inhibit the growth of bacteria or kill them.
What do we mean by resistance to antibiotics?
Bacteria have the natural ability to protect themselves against antibiotics or other microorganisms. Certain genes in the genetic makeup of the bacteria are responsible. These genes are the result of mutations. Bacteria can also share genes and thus pass on resistance. Bacteria can incorporate several of these resistance genes, which then protect them against a number of different antibiotics. The result is multi-resistant bacteria, against which a number of antibiotics are ineffective.